What are normal levels of testosterone?
We’ll talk about the units of measurement usually used in Australia (nmol/l):
- T level under 6: Very low
- T level 6-8: low
- T level 9-11: ‘Down a little’
Blood testosterone levels vary gradually from low to high. So any definition of low testosterone is going to have a best-guess element to it. There is no absolute cut off between low and normal testosterone. Furthermore, the “reference range’ (normal range) is taken from a male age 2o to 40 years of age. Testosterone levels go down by approximately 1% per year. There is an argument for for the “normal ranges” being age-specific rather than single normal range.
A testosterone of 9 or 10 is on the low side for a younger adult male. On the other hand, a testosterone level of 9 or 10 may be acceptable for a male over 70. It’s essential to put put the testosterone level into the whole clinical picture – age, symptoms, weight & medical history.
The Pharmaceutical Benefit Scheme (PBS) allows for prescriptions under medicare. The PBS criteria requires the total testosterone to be less than 8 (with symptoms and signs of androgen deficiency). Testosterone less than 8 is a reasonable figure to distinguish low from normal testosterone but it’s far from the whole story. Indeed, a Testosterone of 12 is low if the LH hormone is significantly elevated.
Please note that Anabolic Steroids push down the measured testosterone level & cause other abnormalities in the blood tests. Testosterone therapy must be avoided to avoid serious complications.
A testosterone level of 9 or 10 may be acceptable for a male over 70
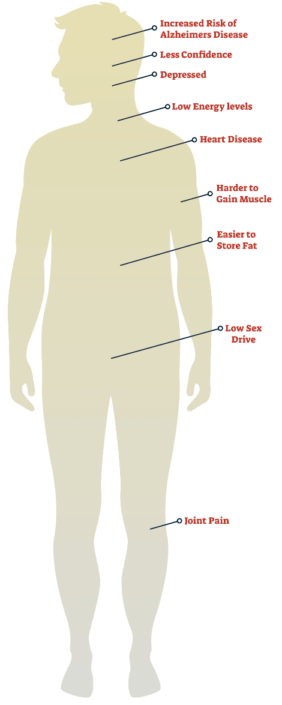
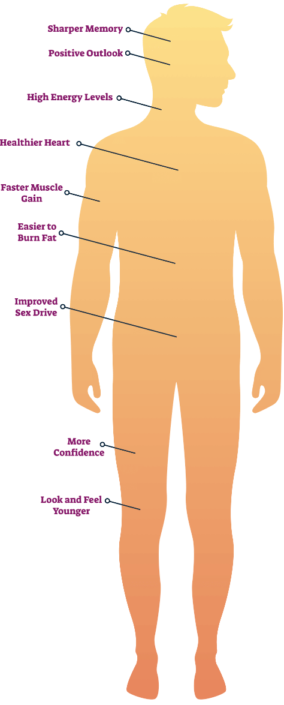
What are the possible benefits of Testosterone Replacement Therapy?
There is evidence that TRT in men with proven androgen deficiency may:
- improve muscle strength
- increase libido
- reduce body fat
- Increase Bone Density
These benefits have been demonstrated from trials of Testosterone therapy on men with clinical hypogonadism (symptoms and signs of low testosterone caused by medical conditions).
Treating guys who simply want to look more muscular is illegal for the doctor. Testosterone became a class 1 drug in Queensland in 2014. In any case, there are definite risks of treating a normal testosterone level.
What about older guys?
This is where it gets more controversial! A landmark study published in the NEJM in 2016 looked at TRT in men age over 65 with a low testosterone. Men were randomly recruited through mass mailings. Men were suitable for the trial if they were over 65 years and did not have conditions like high blood pressure or severe depression. The men were then tested for low testosterone. The cut-off in the trial was a testosterone level of under 8 nmol/l. Low levels were confirmed on a repeat test. Just under 15% of recruits had 2 x testosterone levels under 8 nmol/l. These were the men who participated in the study. In total, 790 men participated in the trial. They were divided into 3 study groups: sexual function, physical function, and energy levels.
Half the men were treated with testosterone gel, and the other half with a placebo gel. Naturally, the men didn’t know which gel they were getting.
What were the results? In those treated with testosterone:
- Libido and erection scores improved.
- Energy Levels did not improve significantly (except in one of the analyses).
- Physical function also improved in one of the analyses.
The study is crammed full of statistics. The bottom line is that there is a modest improvement in sexual performance, and there may be an improvement in physical function or vitality. Results were better when testosterone levels was kept in the upper end of the range.
Australian Society of Autralia included the above trial in their 2016 position statement. In terms of older guys, the main take-home message from their position statement is that many older men with low testosterone have obesity, Type 2 Diabetes or other medical conditions. The society (along with other major guidelines) advocate treating these conditions in order to improve the testosterone.
No-one would disagree with this. The problem is that a significant number of men are unable to sustain long term weight loss without surgery. In the ideal world, the weight should be lost. In terms of TRT, it has to be added that most (62%) of the men in the above testosterone trial had obesity.
What are the risks of Testosterone Replacement Therapy?
There are risks of TRT that are known and/or debated and the following risks are the most important ones.
Cardiovascular Disease risks.
Low Testosterone is associated with an increased risk of cardiovascular disease. However, it is unclear whether this is cause or association. It is currently unknown whether TRT will lower the risk of cardiovascular disease.
There is evidence that TRT might increase the risk of cardiovascular disease particularly when the levels are maintained at the higher end of the normal range. An observational study of pre-existing data in 2014 suggests a doubling of risk of cardiovascular disease in men on TRT who are over 65 years of age. However, this sort of study and others like it are prone to bias. A randomised controlled trial in 2010 of TRT in over 65 year old men had to be stopped early because of a higher risk of cardiovascular events in men on TRT – although the target testosterone in this trial was high-normal at around 17 to 34. On the other hand, the testosterone trial discussed above did not find any increased Cardiovascular risk in the men treated with TRT.
It is certainly prudent, however, to monitor cardiovascular risk in men on TRT – and to aim for a low-normal to mid-normal range.
Prostate Cancer
The prostate gland may be smaller in men with low testosterone. TRT may increase the size of the prostate back to a normal level. Prostate cancer is screened for using the PSA (not a great prostate cancer test but the best widely available medicare subsidised blood test there is). The PSA goes up when the prostate gland increases in size. Therefore, TRT may increase the PSA level. There is no proven increased risk of prostate cancer with TRT based on the data available. The testosterone trial published in 2016 provides further reassurance.
Sleep Apnoea
TRT may exacerbate sleep apnoea.
Raised Haemoglobin levels
Haemoglobin is the oxygen-carrying protein in red blood cells. Testosterone therapy may increase the number of red blood cells which causes a rise in Haemoglobin. An increase in the concentration of red blood cells makes the blood more “sticky” than normal. More sticky blood increases the risk of aterial blood clots which may cause stroke. The Haemoglobin and concentration of red blood cells is monitored during TRT to ensure these remain within safe levels. A ‘haematocrit’ of 0.54 or more would generally indicate the need to stop TRT.
Fertility
Testosterone therapy for “low T” (low testosterone without any disease process) may reduce fertility. On the other hand, TRT may improve fertility in someone with true hypogonadism.
Younger men wishing to have children should be counselled about the risk of Testosterone therapy causing infertility.
The BASHH guideline states that ‘if a man wishes to father children in the near future, then the risk of T therapy on fertility needs to be discussed, because long-term use is associated with azoospermia (absent sperm).’
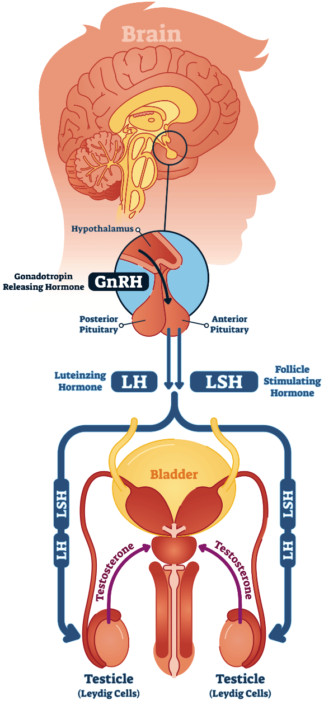
Coming off Testosterone
TRT reduces the production of ‘natural’ T from the Leydig cells in the testicles. In effect, the testicles can ‘shrink’ with TRT.
How long does it take for the testicles to start producing Testosterone again naturally? Clearly, it will take longer for the testicles to ‘recover’ if the testosterone has been taken for a long time, or in high doses. Guys who have taken T from ‘under the counter’ sources for performance enhancement will certainly notice their testicles shrinking.
What are the different types of Testosterone Replacement Therapy?
The different types of TRT are broadly injections and topicals. All of these listed treatments are available under medicare (provided the medicare restrictions are met).
The intramuscular injections are either short acting (eg. Primoteston every 3-4 weeks or so) or long acting (eg. Reandron every 12 weeks or so)
The topical treatments are a convenient way of taking TRT and include:
- Testogel: Gel that is rubbed into the torso or shoulders
- Androderm: Patch applied to back, stomach, thighs or arms
- Axiron: Solution was withdrawn from the Australian market in 2018
- AndroForte cream
Topical treatments may cause skin reactions (particularly the gel and patch) & may be transferred to your partner (gel). Private scripts are more expensive than injections.
The costs of therapy
Medicare raised concerns regarding over-prescribing of testosterone therapy that led to a change of rule in 2015. PBS-subsided prescriptions require initiation by an endrocrinologist or equivalent specialist. There are strong arguments for and against this change of policy, not least the raft of detailed national and international guidelines regarding testosterone therapy. The issue seems to be that some doctors were prescribing testosterone outside of the guidelines.
TRT may of course be prescribed by a doctor outside of medicare, in other words as a private prescription. Clearly, the doctor needs to ensure that the prescription is medically justified. Approximate pharmacy prices for private prescriptions have recently become a little cheaper, and it is possible to pay under $50 per month for one of the topical therapies.
What monitoring of Testosterone replacement is required?
- Symptom Check: is it helping? Therapy takes 1 to 3 months to help. Usually stop testosterone therapy by 6 months if no improvement in symptoms. Are there any side effects?
- Testosterone Blood level: Aim for low-normal to mid-normal adult range. For topical treatments, the level is checked 1-2 weeks following any dose change at the time of day that depends on the brand being used.
- Blood tests: check Haemoglobin, PSA & Lipids/Glucose every 6-12 months
There are other checks that may be indicated: Bone density and sleep studies for example. Guidelines generally advocate an annual prostate exam in the over 50’s taking testosterone.
Symptoms of low testosterone take around a couple of months to improve following replacement therapy.
The aim is to improve symptoms and signs, and not to put the testosterone into a specific range. The therapy should be stopped if there is no improvement following several months of therapy.
Usually stop testosterone therapy by 6 months if no improvement in symptoms
What about my weight?
A weight loss of around 10% in obese men results in an increase in the testosterone level of around 2-3. Major weight loss can increase testosterone levels by more than 10.




Please Telephone us (not email) with any enquiries.